The Longevity Care Battle: Physician vs Digital Platform
#82 Weekly Longevity Medicine Intelligence
Hey Doc,
Welcome to the home of longevity medicine!
What I saw: this week, I watched a revolution in the tech world. Codex, Opus 4.6, OpenClaw, and a wave of AI coding tools changed how millions of people build software, literally overnight. Coding literacy that used to take years to acquire is now accessible to billions of people in a week. It will impact medicine tremendously.
What I heard: More physicians are asking the same question: how do I build a sustainable longevity practice? They want to know about clinical authority, patient experience, protocols, and business models. But there is no playbook but a lot of interest. I also heard from a highly respected physician/researcher who just returned from China. Her assessment: the biotech infrastructure, AI-driven drug discovery, and clinical trial quality she witnessed are now world-class and in some areas, ahead of where we are in the US or EU. The most important breakthroughs in longevity medicine won’t come from one country, they’ll come from physicians who are paying attention globally. Our job is to stay open-minded, explore the cutting edge wherever it emerges, and bring the best of it back to our patients. That’s what forward-thinking medicine looks like.
What I think: Analog care is about to become the ultimate luxury. Not because digital health fails, but because it succeeds and will become the norm. When platforms can automate diagnostics, prescribe medications, and deliver care at scale, the scarcest resource won’t be access, it will be attention. And for the first time in history, doctors now have the tools to practice truly good medicine at scale: data-driven, preventive, personalized. That makes me deeply optimistic.
Happy sunday!
Dr. David Luu - Founder, longevitydocs.™
In this week newsletter:
Cover Story: The longevity care battle: physician vs digital platforms, with 4 investments physicians must make
Research Radar: Publications on lifespan heritability, rapamycin, Lp(a) and vulnerable plaque, urolithin A vs spermidine
Intelligence: Amazon/Lifeforce partnership, retatrutide, Clair hormone monitoring, AI-HIPAA privacy gap
Buzz in the Chat: Physician community debates on retatrutide side effects, and vitamin K2
Community: Shout out to Dr. Joseph Currier our newest CLD (Certified Longevity Doctor)
Each week, I try to explore one idea that could advance longevity medicine and hopefully support physicians in bringing it to life.
The Longevity Care Battle: Physician vs Digital Platform
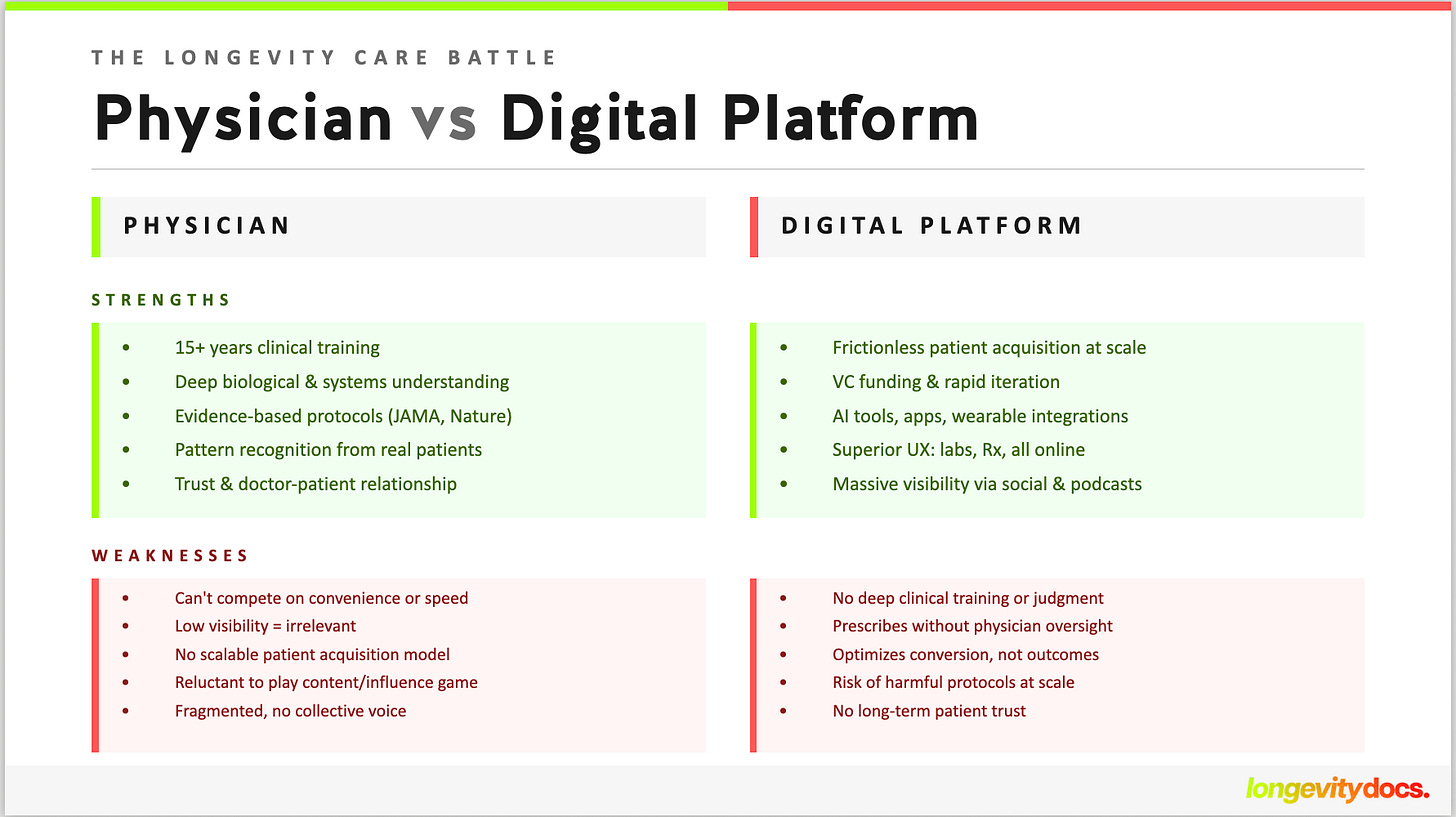
The battle for longevity medicine has begun. On one side: digital platforms armed with venture capital, AI tools, and frictionless patient acquisition. On the other: physicians with 15 years of training, deep clinical knowledge, and a growing sense they’re being outflanked by apps and influencers.
One side optimizes for convenience. The other for clinical rigor. One scales with software. The other depends on relationships. I think there is room for both (if they deliver outcomes)
And if you’re a physician who believes longevity medicine should be led by doctors (not algorithms and checkout carts) you need to understand what’s actually happening, and what you need to do about it.
What platforms got right
In the past five years, digital health platforms launched a revolution. They diagnosed, prescribed, and changed behavior without requiring patients to see a doctor. Most of the time, a simple form was enough.
They had venture capital. They acquired patients at scale. They innovated with apps, tools, and AI. They improved the patient experience. And they filled the gap left by a healthcare system where convenience, access, and cost were never priorities.
Telemedicine platforms proved the model: if you reduce friction, patients will pay out-of-pocket for care that insurance won’t cover and primary care can’t deliver.
Now it’s happening in longevity medicine
What happened in telehealth is now happening in longevity. Platforms are offering MRI scans, advanced labs, wearable integrations, and prescription fulfillment (from statins, ED medications, GLP-1s, compounded hormones, even non-approved research peptides).
The patient journey looks like this: order labs online, upload wearable data, get a prescription, receive supplements and medications by mail. No appointment needed. No physician visit required. Just data in, drugs out.
And the patients? They’re younger than you’d expect. They’re not waiting for their doctor to bring up longevity. They’re getting information from TikTok, friends, and platforms. They’re reading -or at least skimming- research papers. They’re tracking their own biomarkers. They’re looking at outcomes.
Self-care became self-healthcare. And for many, that means physician-less healthcare.
The physician response
On the other side: physicians with updated knowledge, rigorous methods, and clinical training that platforms can’t replicate. They read JAMA, Nature, and The Lancet. They understand biology and medicine at a systems level. They learn from treating thousands of patients.
But they can’t answer the demand. They can’t compete on convenience. And many don’t want to play the visibility game.
One physician said: “I didn’t spend 15 years studying medicine to become an influencer.”
I get it. But here’s the reality: if you’re not visible, you’re invisible. And invisible physicians lose patients to platforms that are visible everywhere: subway, social media, podcast sponsorships, and even SuperBowl ads.
What physicians must do to stay relevant
It doesn’t have to be this way. But staying relevant requires a strategy. Here are the four investments physicians must make:
1. Educate yourself relentlessly
Clinical authority starts with knowledge.
If a patient asks about peptides and your answer is, “They don’t work,” you’ve already lost them. Not because you’re wrong, but because you sound uninformed, dismissive, or outdated.
Patients today are educated, curious, and online.
You need to understand mechanisms.
You need to distinguish between insulin and GLP-1 agonists (FDA-approved, well studied) versus research compounds with limited human data.
You need to explain regulation, side effects, and where the evidence truly stands.
Authority doesn’t mean being defensive.
It means being more informed than the patient and generous with that knowledge.
2. Educate Publicly. Be Visible. Build Trust. Not Followers.
Platforms spend millions educating the market about longevity. They don’t just sell, they shape perception. Physicians must do the same.
Write. Speak. Teach. Explain the science. Break down the mechanisms. Share what you’re learning.
Visibility is not about becoming an influencer. It’s about being discoverable to the patients who are already looking for someone credible.
You don’t need millions of followers. You need a trusted reputation.
In a world saturated with information, trust becomes analog. Patients don’t want a checkout cart. They want to feel heard, understood, and guided.
Be visible but stay grounded. Share your thinking. Share your cases. Stay humble. Keep learning.
3. Build a Circle of Trust. Optimize for Outcomes.
You don’t need to become the loudest voice. You need the best outcomes. That requires collaboration: physician networks, shared protocols, peer-learning, and ethical accountability.
Platforms optimize for acquisition. Physicians must optimize for outcomes.
That’s the moat. That’s the defensibility. That’s what technology can’t replicate.
Build a circle of trust with other physicians.
Review cases together.
Challenge each other.
Raise the standard.
The future: AI democratizes knowledge, not human care
AI will democratize access to medical knowledge. Patients/consumers will have tools that can interpret labs, suggest interventions, and track outcomes. Platforms will get better at personalization, recommendations, and automation.
But AI can’t yet democratize human care. It can’t democratize wisdom. It can’t replace the judgment that comes from treating hundreds of patients. And it can’t replicate the trust that develops when a physician truly understands a patient’s biology, psychology, and life context.
The future of longevity medicine will be deeply rooted in scientific knowledge and human-first care. Patients won’t be uneducated consumers following protocols. They’ll be informed partners expecting collaboration, not paternalism.
That’s where the competition is. Not in who has the best checkout experience. Not in who can ship drugs fastest. But in who can deliver the best clinical outcomes while treating patients as partners, not transactions.
Platforms will win on convenience. Physicians will win on outcomes. I believe the collaboration could actually make the longevity care a really in the next few years.
Every week, the Longevity Docs WhatsApp group feels like a front-row seat to the future of medicine. Here’s what had doctors buzzing:
Retatrutide: is research-grade worth the risk?
A physician asked for guidance after his friend developed generalized cutaneous hypersensitivity without rash a few days after starting retatrutide. The discussion quickly evolved into a broader debate about research-grade peptides versus 503b compounded options, optimal GLP-1 dosing strategies, and when to consider switching from zepbound to retatrutide. Multiple emergency medicine physicians weighed in with real-world side effect data, while others discussed retatrutide’s impressive liver-specific benefits (86% liver fat reduction in phase 2 trials) that distinguish it from pure GLP-1 agonists. The conversation also surfaced growing concerns about long-term glucagon agonism: increased heart rate, amino acid depletion through hepatic catabolism, potential renal hyperfiltration mimicking diabetic nephropathy, and theoretical cardiac myofibrosis through persistently elevated cAMP.
Key takeaways: Retatrutide’s glucagon agonism delivers 86% liver fat reduction but raises long-term safety questions about chronotropic effects, bone health (osteoblast activation), and kidney stress that may take years to manifest
Direct quotes:
“Adding KPV to Reta helps this. It’s a very common reaction. KPV has a local anti-inflammatory effect and mast cell stabilization.” Dr. J
“If targeting the liver specifically, then reta makes sense over Zep. The phase 2 data was staggering up to 86% liver fat reduction in just 48 weeks, with most patients dropping to normal (≤5%) levels. But I refuse to use it until FDA approval. Not a fan of research grade.” Dr. O
“All the serious side effects I experienced in pts that came to my ER were all from pts on max dose (of zepbound). My max is 10mg. And that’s an arbitrary number I created from experience.” Dr. J
About Retatrutide
Clinical & Regulatory Context:
Retatrutide (LY3437943) is an investigational first-in-class triple hormone receptor agonist developed by Eli Lilly that simultaneously activates GIP, GLP-1, and glucagon receptors. Unlike current FDA-approved treatments that target one or two of these pathways (semaglutide targets GLP-1 alone; tirzepatide targets GLP-1 and GIP), retatrutide’s addition of glucagon receptor activation is hypothesized to enhance energy expenditure and hepatic fat metabolism, which is why Phase 2 data showed up to 86% liver fat reduction that distinguishes it from existing agents.
Regulatory status: Retatrutide is not FDA-approved. It is still investigational, meaning it is only available and administered within clinical trials. Eli Lilly’s TRIUMPH Phase 3 program includes multiple ongoing trials, with the first positive readout (TRIUMPH-4) announced December 11, 2025, showing up to 28.7% body weight reduction at 68 weeks. Seven additional Phase 3 readouts are expected in 2026. Eli Lilly is expected to file for FDA approval in late 2026, with potential approval by early 2027.
Safety. The FDA has warned that products sold with labels saying “research peptides” are not intended for human use and should never be self-administered. Online products may contain unregulated powders that are not authentic Eli Lilly compounds, and home mixing raises serious contamination and infection risks. A new safety signal (dysesthesia) emerged in TRIUMPH-4 affecting approximately 20.9% of patients on the highest dose, a finding not reported in earlier Phase 2 trials.
For longevitydocs: Retatrutide’s mechanism is promising and the early data is compelling. But promising mechanism and Phase 3 topline results are not the same as an approved, safety-monitored therapeutic with established dosing, long-term adverse event data, and post-marketing surveillance. Our community’s discussion above reflects exactly the kind of rigorous, evidence-aware clinical reasoning this moment demands: weighing liver-specific benefits against unresolved questions about glucagon agonism, cardiac effects, and renal stress. Until FDA approval, retatrutide remains an investigational compound. Physicians discussing it should do so in that context, and patients seeking it outside of clinical trials are assuming unquantified risk.
For the latest trial data: Eli Lilly TRIUMPH-4 Announcement | ClinicalTrials.gov: NCT05931367
Not a member yet? Join longevitydocs™
We're a physician-only network. Curated. Vetted. Built on trust. If you're committed to practicing longevity medicine with rigor, peer support, and shared standards → this is your community. Apply to connect with our team.
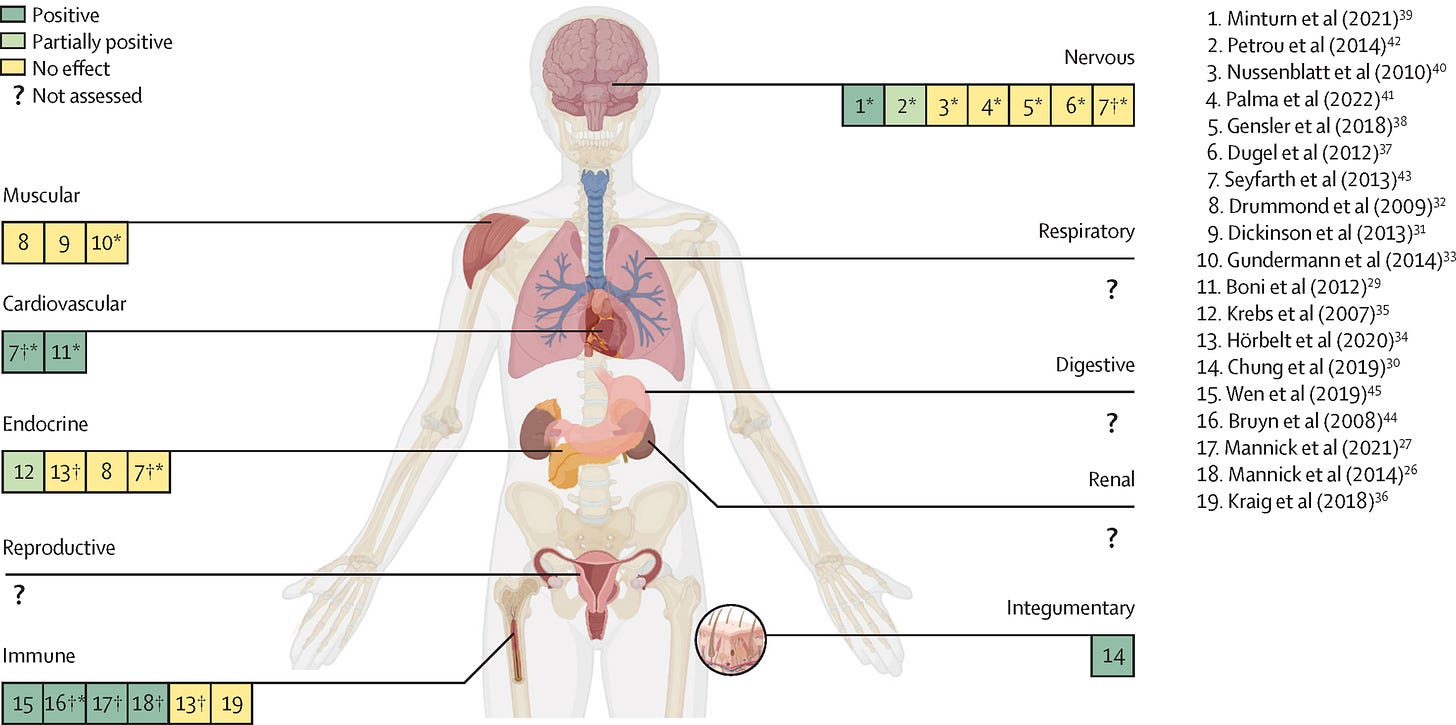
Rapamycin in Humans: What the Evidence Actually Shows
Lancet Healthy Longevity systematic review (Feb 2024) analyzed 19 human studies from 18,400 screened articles on rapamycin and rapalogs for aging. Findings: improved physiological parameters in immune, cardiovascular, and integumentary (skin) systems. No significant effects detected in endocrine, muscular, or neurological systems. Respiratory, digestive, renal, and reproductive systems not assessed. Notably, no clear dose-response relationship emerged across studies, suggesting optimal dosing protocols remain undefined.
For longevitydocs: Human evidence for rapamycin’s anti-aging effects is narrower than the animal data suggests. Before prescribing off-label for longevity, educate your patients that potential benefits might be limited to immune function, cardiovascular parameters, and skin aging, while neurological and metabolic benefits seen in mice haven’t translated to humans yet.
Inherited Risk of Coronary Artery Disease: Redefining Care with Imaging and Genetics
Nature Reviews Cardiology review (Feb 11, 2026) examining how family history captures complex genetic-environmental-lifestyle interplay in CAD risk. Despite high predictive value, family history remains inconsistently defined and under-recorded in routine risk assessment. Authors explore how cardiac imaging and polygenic risk scores can redefine cardiovascular prevention in high-risk families, moving beyond traditional risk calculators to precision assessment combining genomics with structural imaging data.
For longevitydocs: Time to standardize family history assessment and integrate polygenic risk scores + cardiac imaging for patients with premature CAD in first-degree relatives. This precision approach identifies high-risk individuals missed by conventional ASCVD calculators.
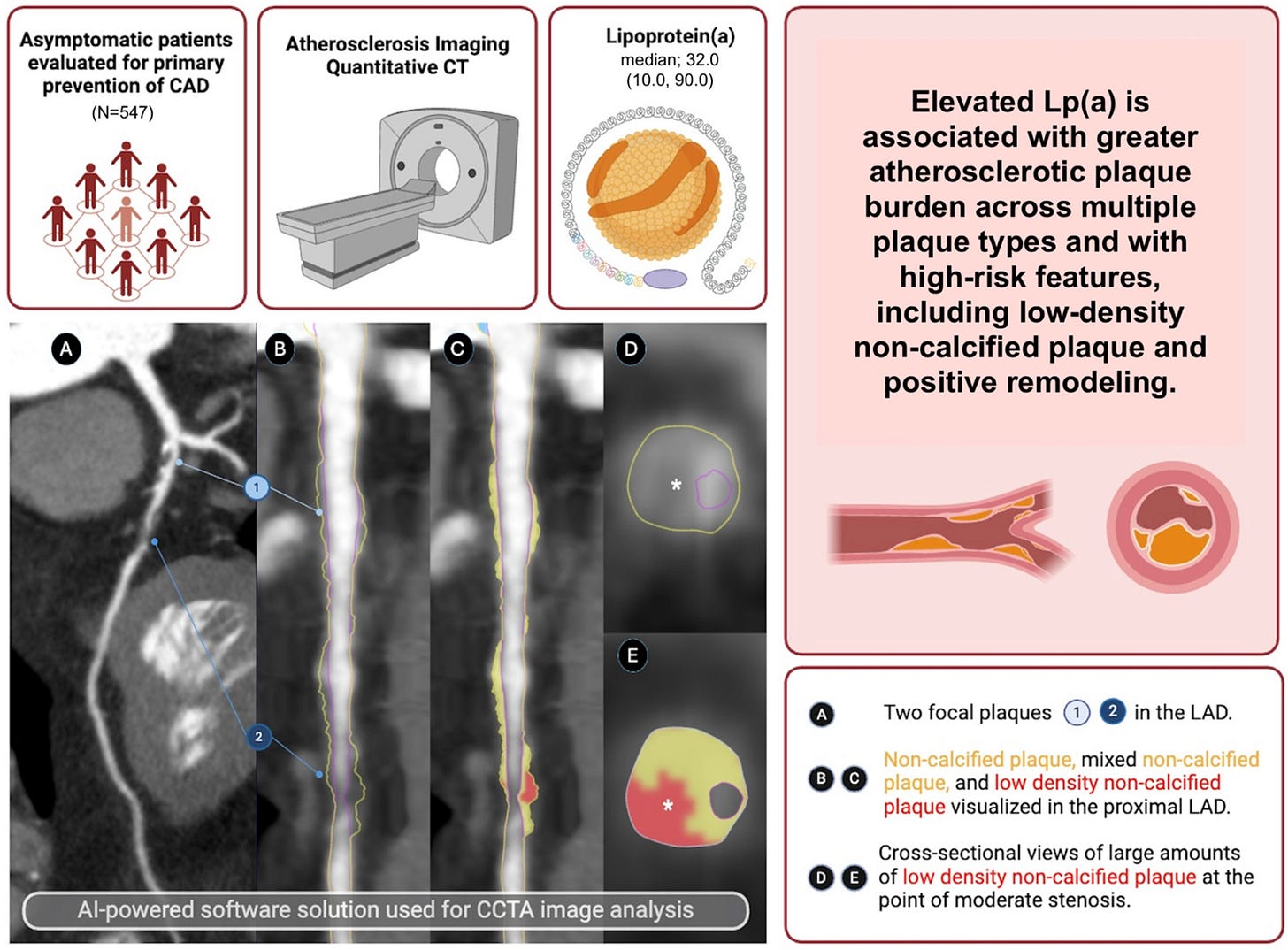
Lp(a) Identifies Vulnerable Plaque That Calcium Scoring Misses
European Heart Journal imaging study (Fisher et al., Jan 28, 2026) analyzed 547 asymptomatic primary prevention patients with AI-guided quantitative coronary CTA. Elevated Lp(a) independently associated with low-density non-calcified plaque (LDNCP) -the vulnerable phenotype most likely to rupture- even after adjusting for age, sex, and other risk markers. CAC score predicted overall plaque burden and calcified plaque (P < 0.000) but showed no association with LDNCP. LDL-P and hsCRP showed no significant plaque associations in multivariable models.
For longevitydocs: Lp(a) and CAC score play complementary roles in risk stratification. For asymptomatic patients with elevated Lp(a) consider coronary AI-CTA even with zero calcium score to assess for non-calcified vulnerable plaque.
European Heart Journal - Cardiovascular Imaging
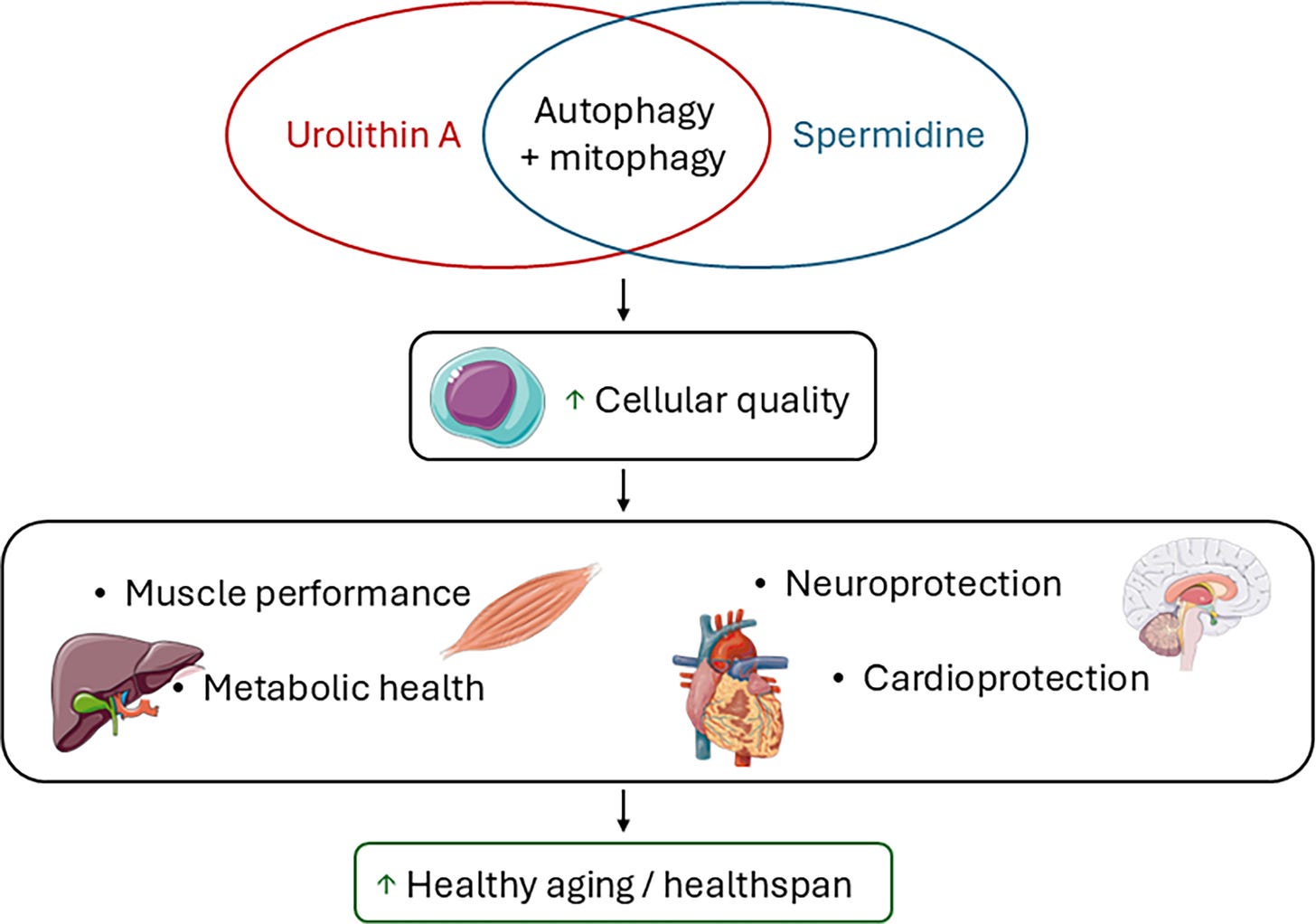
Urolithin A vs. Spermidine: Not All Autophagy Inducers Are Equal
Nutrition Research Reviews comparison (Dec 2025) clarifies distinct mechanisms of two popular longevity supplements.
Urolithin A specifically targets mitophagy via PINK1/Parkin pathway, clearing dysfunctional mitochondria.
Spermidine induces broader autophagy through AMPK/sirtuin 1 regulation
Clinical divergence: preclinical models show urolithin A improves both systolic and diastolic cardiac dysfunction in aging/heart failure; spermidine improved only diastolic function. Human trial (4 months urolithin A) significantly reduced plasma ceramides predicting CVD risk.
For longevitydocs: For patients focused on mitochondrial dysfunction (sarcopenia, heart failure, or metabolic disease with confirmed mitochondrial impairment) urolithin A may be the more targeted choice. Spermidine offers broader cellular maintenance but less specific mitochondrial benefit.
Every week, I track funding, FDA approvals, product launches, and breakthrough announcements shaping longevity medicine.
CARE
Concierge & DPC Models Double, Hitting 7,000+ Providers
Concierge and direct primary care physicians increased 80% since 2018, reaching 7,000+ nationwide twice the predicted growth rate, per Harvard Medical School. While these membership-based models improve physician and patient satisfaction through smaller panels and longer visits, researchers note the system-level cost: fewer doctors available for traditional primary care as burnout drives exodus from fee-for-service models. Harvard Medical School
AI/TECH
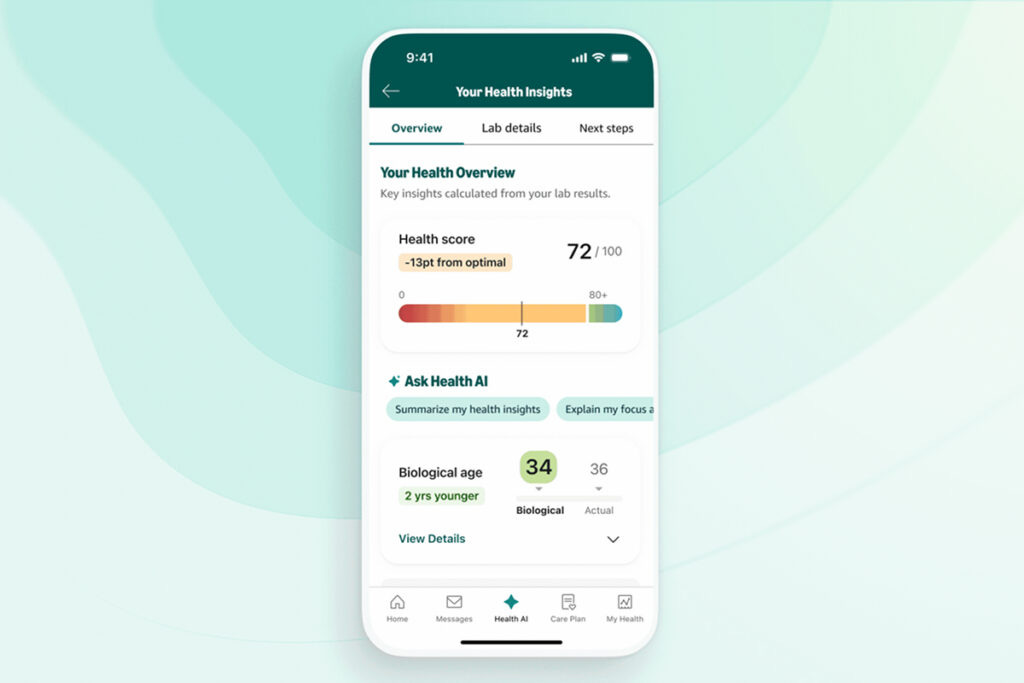
Amazon One Medical Launches Lifeforce-Powered Health Insights
Amazon One Medical launched "Health Insights" (Feb 2026), a beta feature partnering with Lifeforce to analyze 50+ biomarkers from standard bloodwork and generate personalized wellness scores. The app organizes results by health domains (cardiovascular, metabolic, immune) and provides evidence-based lifestyle recommendations. Available at no additional cost to One Medical members.
Clair’s Wearable Infers Hormones Without Blood or Sweat Testing
Stanford startup Clair is launching the first continuous hormone tracker that infers estrogen, progesterone, LH, and FSH from wrist-worn biosensors (no blood draws or sweat analysis required). The device will use AI to triangulate hormonal shifts from 130+ biomarkers including HRV, skin temperature, and sleep patterns, achieving 94.1% cycle-phase accuracy in early validation. Beta launches this month; full device release November 2026.
POLICIES
Your AI Doctor Doesn't Follow HIPAA: Privacy Gaps in ChatGPT Health & Claude for Healthcare
Tech companies like OpenAI and Anthropic almost certainly would not be considered "covered entities" under HIPAA, and they don't claim to be. Anthropic describes Claude for Healthcare as "built on HIPAA-ready infrastructure" (not HIPAA-compliant), while OpenAI's enterprise products "support" HIPAA compliance. ChatGPT Health cannot be made HIPAA compliant since OpenAI won't enter Business Associate Agreements with consumer users. Privacy experts warn: "Assume any information you upload into these tools will no longer be private." Millions are using AI health chatbots without understanding the regulatory gap between consumer AI and traditional healthcare providers bound by HIPAA safeguards. Cyberscoop
Dr. Joseph Currier from ER to longevity Medicine.
Our newest Certified Longevity Doctor (CLD) on why he's starting over and why he's never been more excited about medicine.
After nearly 30 years in emergency medicine, Dr. Joseph Currier is walking away from the ER in April… not because he lost the fire, but because he found a new one.
“Running around ERs for nearly 30 years fixing broken bodies and minds has given me a unique perspective on what is great and what is badly in need of reform with our current medical system. Even after all those years, I still love that job and will always consider it a privilege to care for those on their direst day.”
But the pattern he kept seeing: patients arriving broken, stabilized, and sent back into the same trajectory, changed how he thought about medicine entirely.
“What a novel concept: keep things from breaking. Extend one’s healthspan and worry less about just keeping them alive with multiple comorbidities, chronic pain, limited mobility, and declining cognition.”
Now deep into the CLD training program, Dr. Currier describes the experience with a word you don’t often hear from a physician three decades into practice: excitement.
“I feel like a kid again. As I learn the expansive knowledge base through the Certified Longevity Docs training program, every day I am more convinced that most of our colleagues are still fixed in the old way of thinking. We go to our doctor annually for a brief physical. Check some vitals, maybe a cholesterol and a few basic labs, possibly not even examine you anymore and see you next year. Things look great until they don’t.”
He’s also clear-eyed about the responsibility that comes with the field’s momentum, a point that echoes this week’s cover story directly.
“This justifiable excitement needs to be tempered by our knowledge of the literature and desire to still practice evidence-based medicine. I see this as our crucial role as the landscape spreads throughout social media and into popular culture. Our patients will rely on us to find the best individualized care plan that in many cases may consist of nothing more than foundational principles providing the greatest benefit and lowest cost.”
Dr. Currier doesn’t yet know exactly where he’ll land in the longevity medicine landscape. But his closing line captures something every physician in this community will recognize:
“While I don’t yet know where my place lies in this ever-expanding specialty, I do know I will have a place and am inspired by all of the amazing people I have met already.”
Welcome to the community, Dr. Currier. This is exactly why we built it.
The Certified Longevity Doctor (CLD) program gives you the clinical framework, the evidence base, and the global physician community to make longevity medicine real in your practice.
Next cohort is forming now. Seats are limited.
Mastermind Replays Now Available
3 Masterminds. 3 topics reshaping longevity practice: AI & Tech, Peptides, and Hormones - featuring the dozens of faculty. Trusted by hundred of physicians
If you weren’t in the room, this is your second chance.
Conferences
Feb 19–21 — IH Symposium · New York, NY Integrative health leaders meets
Feb 27–28 — CALM · Fort Lauderdale, FL Clinical approaches to longevity medicine.
Jun 9–11 — Longevity Docs Summit · Cannes, France Our flagship. Physicians, researchers, innovators, investors, policymakers — one stage.
Jun 29–Jul 1 — A4LI H-SPAN Summit · Washington, DC Longevity medicine meets regulation and policy.
Aug 24–28 — ARDD · Copenhagen, Denmark Where aging research meets drug discovery.
Oct 17 — Longevity Docs Skin Longevity Mastermind · New York, NY. Curated physicians. Deep science. One room.
TBA — Longevity Clinics Roundtables · Buck Institute Clinical practice meets research infrastructure.
The Home of Longevity Medicine
longevitydocs.™ is the professional infrastructure for longevity medicine: a physician-only network uniting 600+ physicians across 50+ countries. We build the network, education, research, and culture that make longevity medicine the new gold standard of care.
Longevity medicine is the personalized, evidence-based practice of modifying the root mechanisms of aging (biological, cognitive, and psychosocial) before they become disease, extending healthspan, not just lifespan. Using advanced diagnostics, precision interventions, and AI-enabled monitoring, it translates measurement into action across every medical discipline. Success is measured in functional capacity, vitality, and disease-free years.
Our Pioneering Approach: Network, Education, Research, Culture
Professional Network: A curated, physician-only circle of trust. Leading longevity physicians share protocols, collaborate on clinical challenges, and elevate each other across borders, specialties, and cultures. Shared intelligence as infrastructure.
Medical Education: The Certified longevitydocs™ (CLD) is the first structured, physician-led clinical curriculum for longevity medicine. Comprehensive, evidence-based, and practice-ready. Continuous education programs delivered through structured cohorts and institutional partnerships worldwide.
Clinical Research: A clinical research infrastructure enabling rapid generation of real-world evidence across the longevitydocs™ network. Patient registries, standardized outcome measurement, and multi-center collaboration frameworks that transform everyday practice into coordinated discovery.
Cultural Experiences: From Cannes to New York, our Summits, Awards, Masterminds, and Jefferson Dinners convene top researchers, clinicians, investors, and government officials to shape longevity medicine’s growth, investment, and policy. We write the story of longevity medicine for the world.
Intelligence: Weekly syntheses of scientific breakthroughs, clinical best practices, business signals, and global market analysis; the industry’s trusted source of strategic intelligence for physicians, institutions, and Fortune 500 companies.
Subscribe to the Longevity Docs Newsletter
Longevity medicine is moving fast. Every week, we bring you what matters: clinical insights, research signals, and perspectives from 600+ physicians across 50+ countries. One newsletter. Built for the physicians shaping this field.
Newsletter Disclaimer:

















This is a timely (and very real) framing, Dr. Luu.
What resonated most is your core inversion: platforms will win on convenience; physicians can only win on outcomes + trust. When “labs → algorithm → Rx shipped” becomes frictionless, the scarce resource really does become attention, judgment, and longitudinal context; the things that don’t scale cleanly in software. 
Your four “investments” are also exactly right, especially the nuance that public education ≠ becoming an influencer. It’s about being discoverable and earning trust with coherent reasoning and humility, not volume. 
One “yes, and” I’d add: the differentiator won’t just be physician knowledge, but physician standards—shared protocols, peer review, adverse event reporting, and clear lines between FDA-approved therapeutics, compounded meds, and research compounds. If platforms optimize for acquisition, the physician moat is governance + outcomes. 
Also appreciated the line that feels almost prophetic: “Analog care is about to become the ultimate luxury”, not because digital fails, but because it succeeds. That’s an uncomfortable truth, and a useful one for anyone building a longevity practice right now.
Thanks for the shoutout! Thrilled to be a part of it.