The AI Doctor Is Born
#77 Weekly Longevity Medicine Intelligence
The AI doctor was born this year, not in a hospitaI.
I was at CES to speak about longevity medicine and technology, and what I saw was clear: AI, robots, and digital health are no longer being built for medicine. They are being built as medicine: designed to improve health, extend life, and redefine how care is delivered.
I’m deeply grateful to represent longevitydocs and to speak on the stage of one of the world’s most influential technology conferences, seeing longevity medicine recognized as a legitimate field and a movement of the future.
The convergence of longevity medicine and technology is no longer theoretical. It’s here. And it’s an extraordinary moment to be part of this revolution alongside the physicians and innovators shaping what comes next.
Dr. David Luu - Founder, longevitydocs.™






Each week, I try to explore one idea that could advance longevity medicine and hopefully support physicians in bringing it to life.
The AI Doctor Is Born
What It Means for longevitydocs, and Why Physicians Must Lead This Transition
The AI doctor didn’t arrive with a white coat or a press conference. It arrived quietly, and soon it will be everywhere.
ChatGPT for Healthcare is analyzing patient data and citing medical literature. Function is integrating lab results into consumer AI tools. Doctronic is prescribing medications autonomously in Utah. AI is now serving patients directly through analysis, education, and now prescription.
But AI isn’t just for patients. It’s already embedded in how physicians work: notes, workflows, clinical decision support, and increasingly, patient care itself. Doctors are using it whether they’ve formally adopted it or not.
For longevity medicine, AI is not optional: it’s mandatory.
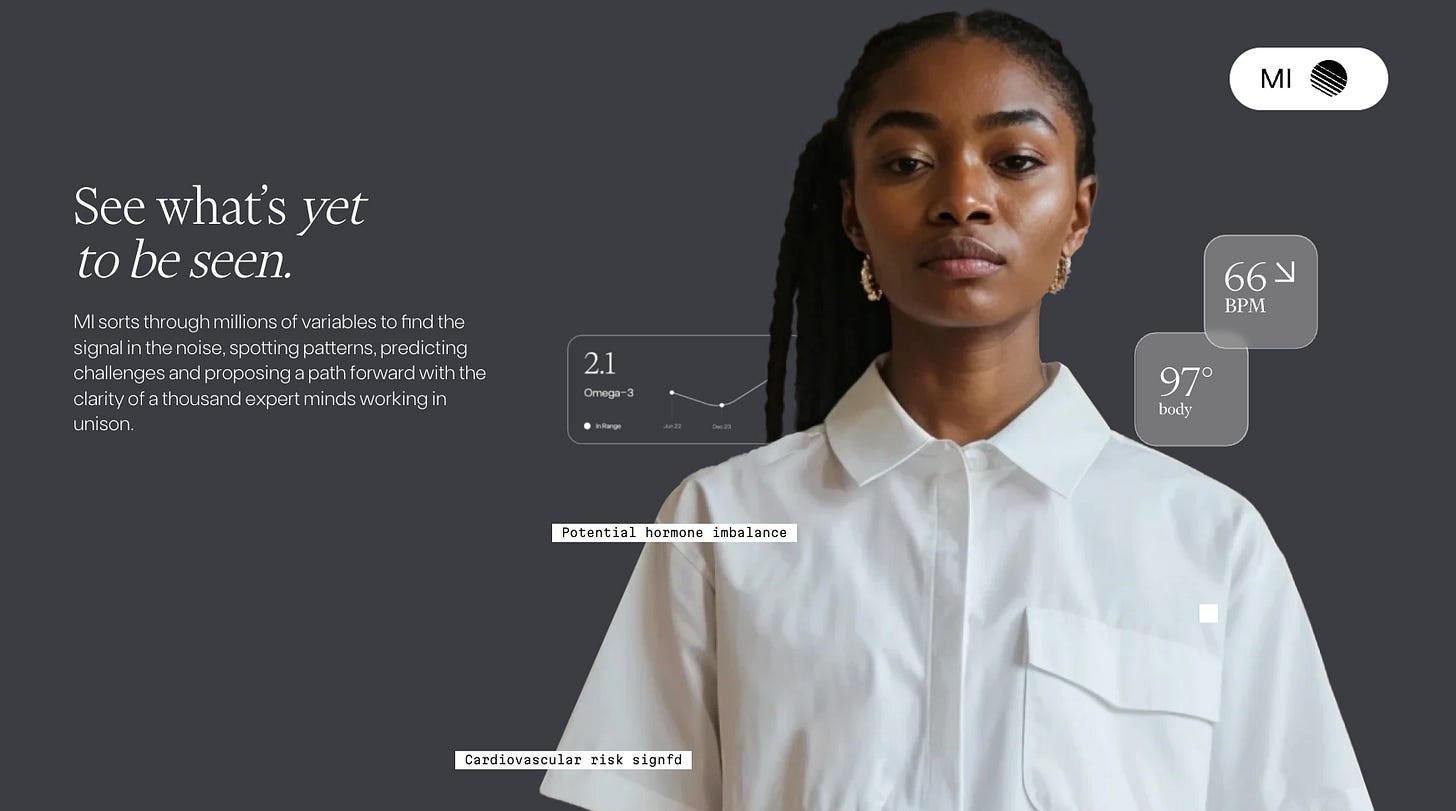
Longevity care is longitudinal, preventive, and inherently data-heavy. It requires detecting weak signals early, tracking trajectories over time, and integrating biology with behavior, environment, and lifestyle.
We’re working with multi-omics, advanced imaging, continuous lifestyle data, and interventions that span every organ system and aging pathway. No single physician -no matter how experienced- can manually process, synthesize, and monitor all of this in real time.
AI becomes the infrastructure that makes modern longevity medicine possible, while the physician remains the one who interprets, decides, and guides.
The 5 Biggest Opportunities for Longevity Medicine
1. Earlier Signal Detection Across Aging Pathways
Subtle shifts in inflammation, metabolic flexibility, sleep architecture, hormonal balance, or mitochondrial function are almost impossible to track manually across time and systems. AI excels at longitudinal pattern recognition across organs and pathways, exactly where early intervention matters most in longevity medicine.
2. N-of-1 Precision at Scale
AI makes it possible to practice true personalized longevity medicine at scale. By continuously analyzing labs, wearables, imaging, multi-omics, and lifestyle data over years (not single visits) AI allows physicians to track individual biological trajectories and deliver N-of-1 care without sacrificing precision as practices grow.
3. More Time for Clinical Judgment and Human Care
By automating intake, synthesis, and documentation, AI frees physicians to focus on what cannot be automated: interpretation, strategy, motivation, context, and trust. The longevity doctor shifts from data processor to clinical architect.
4. Expanded Access to Longevity Expertise
Hybrid AI + physician models allow longevity doctors to serve more patients without compromising standards, critical as demand for preventive and longevity care continues to outpace supply.
5. Stronger Clinical Consistency
Used correctly, AI can reinforce evidence-based care, reduce unnecessary variability, and support best practices - while still allowing physicians to personalize decisions based on biology, goals, and risk tolerance.
The 5 Risks Longevity Docs Must Take Seriously
1. Patient Confusion and Data Overload
More data is not always better. AI-generated summaries can overwhelm patients, amplify benign abnormalities, and drive anxiety without proper physician framing.
2. Overtesting and Overintervention
Large panels can increase false positives. Without restraint, AI-driven insights can push patients toward unnecessary supplements, testing cascades, or interventions.
3. Deskilling of Physicians
Over-reliance on AI risks weakening first-principles clinical reasoning. Longevity doctors must remain deeply fluent in biology, not passive reviewers of algorithmic output.
4. Governance, Privacy, and Liability Gaps
HIPAA, BAAs, data ownership, consent, and liability remain unresolved in many AI deployments. If AI makes a mistake, responsibility is still human and unclear.
5. Premature Autonomy
AI is not ready to independently diagnose or treat complex, multi-system longevity patients. Moving too fast risks harm, regulatory backlash, and erosion of trust.
What Longevity Docs Should Do Now
The opportunity is real. The risks are serious. But waiting is not a strategy. Longevity physicians must act now—not by rushing to adopt every new tool, but by leading with intelligence, discipline, and a clear plan.
1. Educate and Train Your Team
AI literacy is now clinical literacy. Physicians and staff need to understand what AI can do, what it cannot do, and where human judgment remains non-negotiable. This means training on:
How AI tools work and where they fail
Interpreting AI-generated outputs critically, not passively
Explaining AI recommendations to patients clearly and accurately
Recognizing when AI is creating noise instead of signal
Education isn’t a one-time event. It’s an ongoing commitment as tools evolve and new capabilities emerge.
2. Assess Accuracy and Clinical Validity
Not all AI tools are created equal. Before integrating any AI system into your practice, you must assess:
Clinical accuracy: Does it perform well in real-world longevity populations?
Evidence base: Is it built on robust data or marketing claims?
Transparency: Can you understand how it arrives at recommendations?
Failure modes: What happens when it’s wrong, and how will you catch it?
Longevity patients are complex and don’t fit clean diagnostic categories. Any AI tool used in this space must be validated for the populations you serve, not just tested in general medicine cohorts.
3. Build Your Own Model or Partner with the Right Tech Companies
Longevity doctors have two paths forward: build proprietary AI systems tailored to your practice, or partner with technology companies that align with your clinical values.
If you build, you control the data, the algorithms, and the integration—but you also own the risk, cost, and operational complexity.
If you partner, choose carefully. Look for companies that:
Prioritize clinical outcomes over efficiency metrics
Offer transparent governance and HIPAA-compliant infrastructure (including BAAs)
Allow physician oversight and the ability to override recommendations
Are willing to co-develop solutions with clinicians, not just sell to them
The worst outcome is passive adoption: letting platforms, payers, or influencers decide how AI gets deployed in longevity care. If physicians don’t lead this transition, others will.
AI is not coming to longevity medicine. It’s already here.
ChatGPT is analyzing patient data. Function is integrating labs into AI tools. Doctronic is prescribing medications. The era of AI-augmented care has begun.
For longevity doctors, this is not a threat. It’s a responsibility. The doctors who engage with AI thoughtfully -who educate themselves, assess tools rigorously, and build or partner strategically- will define how longevity medicine scales. Those who wait will lose influence over how care is delivered.
The future of longevity medicine won’t be built by algorithms alone but by doctors who know how to use them.
If you want to be in the room shaping AI-powered longevity care, join our AI & Tech Mastermind in NYC · January 31.
Every week, the Longevity Docs WhatsApp group feels like a front-row seat to the future of medicine. Here’s what had doctors buzzing:
Rapamycin & Ovarian Aging: “Promise, Protocol… and Patient Selection”
A fertility thread lit up the chat: a patient wanted rapamycin for fertility.
What doctors said
What emerged:
Typical dosing being discussed: 5–6 mg once weekly, often cycled (ex: ~3 months on, ~2 months off, repeated)
Outcomes are mixed: some clinicians use it for ovarian aging strategies; others report minimal fertility signal, including no AMH improvement in select cases
Side effects: muscle loss, depressive symptoms, and metabolic changes were raised as real barriers
Clinical reality: fertility goals + off-label geroscience meds = high uncertainty, so consent, monitoring, and stop-rules matter
Comparison point raised in the chat: some physicians feel GLP-1s may be a better “balanced” lever on overlapping aging axes (still not a fertility drug, but clinically familiar and more physiologic in mechanism)
One line captured the spirit of the thread:
“If AMH doesn’t budge and quality of life drops, the protocol is failing, even if the theory is beautiful.”
Key Takeaway: Rapamycin in fertility isn’t “pro” or “anti.” It’s personalized medicine. Dosing is easy; patient selection, monitoring, and managing downside risk is the work.
GLP-1s in Longevity Practice: “Plateaus Aren’t Failure, They’re a Signal”
A patient plateaued. Microdosing came up.
Storage and “how long is the vial good?” became the real-world problem.
What emerged:
Plateau ≠ nonresponse: clinicians pushed for body composition over scale weight (DEXA/InBody) and asked, “Are they losing fat or losing momentum?”
Microdosing creates new operational questions: leftover medication, refill timing, and how long patients are drawing from the same vial (especially when use is off-label)
Side effects can be the limiting factor: reports of pimples / skin changes, canker sores / mouth sores, and tolerability issues that become adherence barriers
Mechanism matters: plateau discussions quickly moved to mitochondrial function and substrate metabolism
One line captured the thread:
“If they’re exhausted and not moving, the medication is working against us.”
Key Takeaway: GLP-1s are now systems medicine. Plateaus demand better measurement (fat vs lean), better ops (vial use, cadence), and better physiology (mitochondria, activity, gut-mediated metabolites) → not reflex escalation.
ChatGPT for Healthcare: “Power Tool, Not Autopilot”
An AI thread split into two camps fast: some saw relief, others saw risk.
A new “healthcare-grade” ChatGPT product was shared.
People asked about HIPAA.
Then one question grounded everything:
Do they have a BAA?
What emerged:
Upside is real: faster evidence navigation, documentation support, triage, and administrative relief… if implemented correctly
But governance is the whole game: clinicians flagged the need for BAA, clear policies, and understanding where data goes, who stores it, and who can access it
Patient impact is nontrivial: multiple docs reported that ChatGPT can confuse and overwhelm patients, especially when outputs are confident, verbose, or poorly contextualized
Privacy nuance came up: if patients “upload themselves,” the risk profile differs than when a third party stores and shares data
Cultural risk: a critical take was shared warning that healthcare AI can become a marketplace where incentives drift away from patients unless physicians lead implementation
One line captured the thread:
“The risk isn’t AI… it’s AI without a grown-up in the room.”
Key Takeaway: AI can be transformative for doctors only if it’s wrapped in HIPAA-grade governance (BAA, data controls, audit trails) and used to augment clinical reasoning, not replace it or flood patients with unmanaged information.
Not a member yet? Join the debate in the WhatsApp group
Longevity Docs is a highly vetted, invitation-only community for physicians shaping the future of longevity medicine. Apply to connect with our team.
Faculty & Agenda: AI & Tech Mastermind (part 1)
We've curated a world-class faculty of physician-scientists and clinical leaders who are defining the future of longevity medicine. Each session is designed to bridge cutting-edge science with immediate clinical application - giving you the tools, evidence, and protocols to integrate these advances into practice now.
The Aging Clocks Menu
What clocks physicians should order to guide longevity interventions
David Furman, PhD
Dr. Furman is Director of the Stanford 1,000 Immunomes Project and Chief of AI at the Buck Institute for Research on Aging, where he pioneered the inflammatory aging clock (iAge) used in clinical longevity practices worldwide. His work bridges systems immunology, machine learning, and translational medicine—with over 20 patents and publications in Nature Medicine, Cell, and The Lancet.
The Multi-Omics Protocol
pTAU-217, Mitochondrial Function, Proteomics, Metabolomics: Which Tests Are Actually Worth It?
Steve Murphy, MD
Dr. Murphy is a practicing family physician who runs a precision longevity practice built on multi-omics testing, including proteomics, advanced mitochondrial panels, pTAU biomarkers, and metabolomics. He's known for helping physicians navigate which next-gen tests are clinically actionable today versus which are still research-grade - and for building practical protocols that improve patient outcomes without creating data overload.
The SkinSpan Stack
Your Patients Are Already Using ViziaScan and Skin Age Clocks - Here's What Actually Works
Saranya Wyles, MD, PhD
Dr. Wyles is Director of the Regenerative Dermatology and Skin Longevity Laboratory at Mayo Clinic and holds an M.D., Ph.D. in Regenerative Medicine. She's leading clinical trials on platelet-derived exosomes for skin rejuvenation, topical senolytics for chronic wounds, and 3D bioprinted skin models to target cellular senescence—translating regenerative technologies from discovery to clinical application in longevity dermatology.
Zoom on Cardio Longevity
The Most Advanced Cardiovascular Biomarkers for Longevity Clinics
Giovanni Campanile, MD
Dr. Giovanni Campanile is a quintuple board-certified cardiologist and a pioneer in integrative cardiology, combining conventional heart care with holistic, lifestyle-based approaches, focusing on prevention and disease reversal through nutrition and integrative therapies. He's known for directing significant cardiac rehab programs (like the Ornish program), researching at the Framingham Heart Study and serving as a medical writer. Dr. Campanile has published scientific papers in major cardiology journals that have advanced our understanding of the effect of high blood pressure on heart health. He also started the very first Integrative Cardiology practice in the nation.
Agenda:
The AI Grand Replacement
Are Physicians Next Or Is This Just Another Technology Tool?The Aging Clocks Menu
What physicians should order to guide longevity interventionsThe Multi-Omics Protocol
pTAU-217, Mitochondrial Function, Proteomics, Metabolomics: Which Tests Are Actually Worth It?Zoom on Cardio Longevity
The Most Advanced Cardiovascular Biomarkers for Longevity ClinicsCase Study: AI-enhaced Longevity Doctor
How AI Can Improve Patient Outcomes, Increase Revenue, and Reduce BurnoutScaling Longevity Clinics with AI
From 100 to 1,000 Patients - Is It Possible Without Sacrificing Quality?How to Build an AI assisted clinic
Heads UpHow to Implement an AI EHR
Vibrant PracticeAI-powered decision support tools
LongevitixThe SkinSpan Stack
Your Patients Are Already Buying ViziaScan and Skin Age Clocks - Here’s What Actually WorksThe Neuro tech game
Advanced Tools for Mental Health, Dementia, and Cognitive Performance - What’s Ready for Clinical UseConnected Longevity
Wearables, Continuous Monitoring, AI Predictions - Which Data Actually Changes Clinical Decisions?
Small group. Curated. Limited to 150 Physicians only.
VIP (50 spots) - Includes private dinner with speakers
In-Person (limited) - Full access to all sessions and networking
Virtual - Live-stream and replay for those who can’t travel
Anti-aging strategies and ex vivo organ rejuvenation
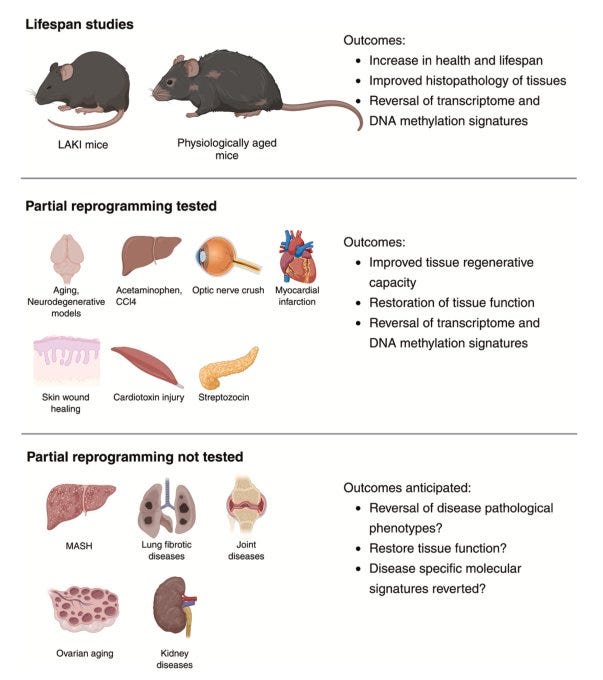
Aging is characterized by a progressive decline in physiological function, driven by interconnected molecular hallmarks that increase the risk of chronic diseases. To extend health span, interventions targeting these hallmarks, including lifestyle modifications, pharmacological agents, and genetic strategies, have been developed. Among these, partial reprogramming, the transient expression of Yamanaka factors, has emerged as a powerful approach to reverse age-related cellular damage and restore youthful epigenetic and transcriptional signatures without erasing cell identity.
A multimodal sleep foundation model for disease prediction
A new foundation AI model, SleepFM, trained on 585,000+ hours of polysomnography from ~65,000 patients, shows that one night of sleep can predict long-term disease risk, accurately forecasting 130 conditions including all-cause mortality, dementia, myocardial infarction, heart failure, stroke, CKD, and atrial fibrillation (C-index up to 0.85); for doctors, this is powerful because it reframes sleep from a symptom to a high-resolution biomarker of systemic aging and disease risk, but it also signals caution: translating complex, black-box risk predictions into actionable, ethical clinical decisions will require strong validation, patient education, and physician-led interpretation — not automation alone.
Every week, I track funding, FDA approvals, product launches, and breakthrough announcements shaping longevity medicine.
AI/TECH
ChatGPT unveils new health tool for doctors
OpenAI launched ChatGPT for Healthcare, a HIPAA-aligned, physician-tested AI suite that integrates with clinical systems and cites peer-reviewed evidence; it’s promising for doctors because it can reduce administrative burden, speed up evidence synthesis, and support more personalized care, but it requires vigilance since AI can still propagate errors, oversimplify complex clinical decisions, or be deployed for efficiency over patient-centered care without strong physician governance.
Function launches AI doctor in your pocket
Function launched a new app inside ChatGPT, allowing members to securely authorize access to a limited, high-level summary of their lab results so ChatGPT can deliver more personalized health responses; this is meaningful because it signals a shift from generic AI advice to context-aware health guidance, but it also raises important considerations around data governance, patient understanding, and the need for physician oversight as lab-driven insights increasingly flow directly into consumer AI tools.
POLICIES
Artificial intelligence begins prescribing medications in Utah
Utah is piloting AI-only prescription renewals with Doctronic, removing physicians from routine refills for select chronic meds; this is attractive for doctors because it can reduce refill fatigue, lower costs, prevent medication lapses, and triage truly complex cases back to clinicians, but it demands caution since autonomous prescribing raises safety, misuse, and liability risks, tests patient trust, and pushes regulation ahead of consensus — making physician oversight, escalation rules, and clear accountability essential.
PHARMA
Chinese Peptides’ Are the Latest Biohacking Trend in the Tech World
A growing tech-driven trend dubbed “Chinese peptides” shows Silicon Valley users sourcing unregulated, unapproved peptides directly from China to self-inject for weight loss, cognition, sleep, and performance, bypassing physicians and the FDA; for doctors, this matters because patients are increasingly experimenting ahead of evidence, extrapolating from GLP-1 success to dozens of untested compounds, creating real risks around contamination, misuse, addiction, and missed diagnoses — and reinforcing the urgent need for physician-led education, boundaries, and harm-reduction conversations rather than silence or dismissal.
SOCIETY
The Rise of the Self-Serve Blood Test
The New York Times examines the rise of self-serve blood testing platforms like Function, which offers hundreds of lab markers without a physician visit, appealing to patients who feel ignored by traditional medicine and want proactive, data-driven insight; for doctors, this trend matters because while expanded testing can validate symptoms and surface early risk signals, it also increases false positives, anxiety, supplement overuse, and interpretation gaps when clinicians aren’t involved early — reinforcing the need for physician-led context, restraint, and clear guidance on what data actually warrants action.
Supplements Are a $70 Billion Industry. RFK Jr. Is Good for Business.
The WSJ reports that Robert F. Kennedy Jr.’s rise is a tailwind for the $70B U.S. supplement industry, as his rhetoric about “ending the war on vitamins” and alignment with wellness influencers normalize pills, powders, peptides, and IV drips that bypass FDA approval; for doctors, this matters because consumer demand is accelerating faster than evidence or regulation, blurring lines between prevention, treatment, and marketing — increasing the need for clinician-led guidance, conflict-of-interest awareness, and clear patient education on what supplements can (and cannot) safely do.
The world’s largest physician network in longevity medicine
longevitydocs.™ is the world’s largest physician network in longevity medicine, serving 600+ vetted physicians across 50+ countries. We unite physicians, industry, and institutions to build the trusted global infrastructure that makes longevity medicine the new standard of care.
Longevity medicine is the personalized, evidence-based practice of modifying the root mechanisms of aging (biological, cognitive, and psychosocial) before they become disease, extending healthspan, not just lifespan. Using advanced diagnostics, precision interventions, and AI-enabled monitoring, it translates measurement into action across every medical discipline. Success is measured in functional capacity, vitality, and disease-free years.
Our Pioneering Approach: Uniting Science, Clinical Practice, and Culture
Professional Network
Global Longevity Community: A curated community of leading longevity physicians fostering peer learning, clinical collaboration, and professional growth
Medical Education
Certified longevitydocs.™ (CLD): The first structured, physician-led clinical curriculum for longevity medicine - comprehensive, evidence-based, and practice-ready.
Clinical Research
Longevity Research Network: Clinical research infrastructure enabling rapid generation of real-world evidence across the Longevity Docs network.
Cultural Experiences
Global Events: From Cannes to New York, our Summits, Awards, Masterminds, and Jefferson Dinners convene top researchers, clinicians, investors, and government officials to shape longevity medicine’s growth, investment, and policy.
Intelligence
Strategic Insights: Weekly syntheses of scientific breakthroughs, clinical best practices, business signals, and global market analysis for Fortune 500 companies - the industry’s trusted source of intelligence.
Not a member yet? Longevity Docs is an invitation-only network of 600+ physicians shaping the future of longevity medicine through clinical collaboration, certification, and global events.
Subscribe to the Longevity Docs Newsletter
Stay connected with a global network of 500+ physicians in 50+ countries advancing longevity medicine. Get evidence-based insights, clinical updates, and exclusive access to the community shaping the future of longevity care.
Newsletter Disclaimer:


















I'm so stoked about AI in medicine. I was talking to a dude getting his phd in it. They're working on implementing AI in hospitals wide spread. SO DOPE
This is such a grounding way to name what so many people feel in December: it’s not “you being dramatic”, but it’s a cultural stimulus package that reliably activates stress physiology; scarcity pressure (money/time), social evaluation, family dynamics, sensory overload, and a manufactured “perfect togetherness” standard that no nervous system can sustainably perform. I also really appreciate the Jungian “complex” framing because it maps onto modern clinical reality: when the script is activated, people aren’t just having thoughts, they’re having state changes (sleep disruption, irritability, urgency spending, appetite shifts, shutdown). Bringing the pattern into awareness is often the first step toward regulation.
The most practical takeaway here for our longevity-focused readers is exactly what you outline: interrupt the loop with something bodily (walk, breath, stretch, delay the purchase, step out of the retail environment), then make one values-based choice; one boundary, one simplified tradition, one “good enough” gift decision. That’s not small; that’s nervous-system leadership!
Thank you for making this feel both psychologically precise and deeply humane—especially for those who don’t even celebrate Christmas but still have to live inside the season.