From Barber To Longevity Doctor
#80 Weekly Longevity Medicine Intelligence
Hey Doc,
Sundays are always a great time to reflect. Exactly a year ago I was coming from Davos where we hosted an inaugural discussion on longevity medicine. I am grateful for the amazing community and ecosystem we built in a year. Especially how much more mature the field became. "Longevity Medicine" is globally discussed, challenged, and gathering more physicians who are excited to learn and connect to treat patients better.
I talked to dozens of doctors in our certification program and it was very cool to hear them say:
“It’s refreshing to finally have a physician-only, physician-led space. That alone makes a difference.”
“This feels like a new layer of medicine that every specialty can add on top of what they already do.”
“I needed to be excited about learning medicine again and this did that.”
“Longevity Docs feels like the right community for physicians who want to practice preventive and precision medicine seriously.”
“You’ve created a hub where physicians interested in longevity can actually find each other.”
It give us the community, the team, the ecosystem to keep believing in our mission.
Medicine has always evolved. The science evolves. The therapies evolve. The technologies evolve. Our role has evolved from barber-surgeon to specialist to digital scribe.
Now we evolve again.
PS: Stay warm if you are in the storm… or go skiing ;)
Dr. David Luu - Founder, longevitydocs.™
Each week, I try to explore one idea that could advance longevity medicine and hopefully support physicians in bringing it to life.
From Barber to Longevity Doctor
Do we have to reinvent ourselves?
As physicians, we’ve spent decades mastering our craft. Now, technology is reshaping everything we thought we knew about how medicine works.
But this isn’t the first time.
In the 1500s, doctors were barber-surgeons: craftsmen who cut hair and amputated limbs.
The 1800s brought germ theory and medical schools, transforming us into diagnosticians.
The 1900s fragmented medicine into specialties, making us technicians.
The 2000s turned us into digital scribes, typing while patients talked, drowning in EHRs.
Each era demanded reinvention. Each time, we feared obsolescence. Each time, we emerged more essential, not less.
Now we’re at another inflection point.
Imagine a world where laboratory testing becomes a commodity.
Where data is monitored continuously.
Where AI analyzes signals in real time: flagging rising cardiovascular risk and detecting diseases of aging before symptoms ever appear.
In that world, what is the role of the doctor? Are we still part of the equation?
I was listening to Jensen Huang on a panel saying that radiologists are busier than ever; precisely in a field where many assumed AI would replace them. Instead, AI allows them to read more images, faster and with greater accuracy. Productivity increases. Access improves. Clinical judgment becomes more valuable, not less.
In a world where physicians are becoming scarce (who wants to get into med school and debt - in the US), improving productivity is not optional if we want to care for more patients, not fewer.
Now imagine the near future.
A patient is referred to you but because AI identified you as the best fit for her profile. She arrives with her labs, imaging, and functional testing already completed at a longevity hub. A digital twin has modeled her risks and proposed evidence-based interventions and therapies.
So what is your role?
More human than ever.
Today, doctors are stepping into a new function, one patients are actively seeking. Technology handles the volume, the monitoring, the pattern recognition. Physicians are finally free to practice the art of medicine again.
The new roles of the longevity doctor:
The Educator: translating complex science of aging into actions
The Guide: helping patients navigate choices and trade-offs
The Analyst: validating insights, challenging assumptions, applying clinical judgment (based on decades of expererience)
The Motivator: supporting behavior change months over month, listening, motivating
Human consultation will become a luxury: not because it is rare, but because it is deeply valuable. Technology will democratize access to high-quality longevity care; physicians will elevate it.
We must be ready for this transition.
Ready to train the next generation.
Ready to empower patients to take ownership of their health.
One physician recently told me:
“I’m building a community, not just to treat my patients, but to educate them, understand them better, and support them over time.”
AI will not dehumanize medicine.
If we do this right, it will finally allow medicine to become what it was always meant to be:
Preventive. Personalized. Human.
This is why Longevity Docs exists: to help physicians build the infrastructure that makes longevity medicine the new standard of care.
If you're ready for this shift, join us in NYC on January 31. Small group. Real doctors. Honest conversations about where medicine is headed.
Every week, the Longevity Docs WhatsApp group feels like a front-row seat to the future of medicine. Here’s what had doctors buzzing:
GLP-1 + thyroid cancer: rodent warning ≠ human signal
The SLU-PP thread spilled into GLP-1 risk discussion—specifically the “family history of thyroid cancer” question. The group pushed back hard on blanket contraindications, pointing to mechanism differences and real-world epidemiology.
Are we over-indexing on the black box warning and under-treating cardiometabolic risk?
Key takeaways
The MTC warning is largely rodent-driven.
The group emphasized differences in GLP-1 receptor expression between rodent vs human C-cells.15+ years of real-world use matters.
Clinicians cited millions of patients without a clear epidemiologic signal of medullary thyroid cancer.Calcitonin monitoring is happening in practice.
Some physicians track calcitonin quarterly / multiple times per year and reported no meaningful movement.Consent strategy is nuanced.
Some don’t include MTC as a prominent consent risk, but do explain the black box and why the human relevance appears limited—framed as defensible with existing data.
“We’re using compounds with no safety data… and then worried about a GLP-1 that has no mechanism or evidence of cancer.”
Exosomes: topical is “cleaner,” injectable is the wild west
Exosomes triggered one of the most “regulation vs reality” conversations of the week. The distinction between topical use, device-assisted delivery, and injection came up repeatedly - along with Korea/Japan claims and what “on-label” even means in practice.
Are clinics accidentally building protocols on regulatory sand?
Key takeaways
Injectable exosomes: widely used, poorly standardized, often off-label.
The group emphasized that approved injectable exosome products are not broadly established in many markets.Topical/device-assisted use sits in a different category.
RF microneedling / fractional / pico + topical exosomes were discussed as a more “label-aligned” route for certain settings.“Plant exosomes” vs plant stem-cell derived vesicles: terminology gets sloppy fast, and why precision matters when you’re designing protocols or studies.
Korea/Japan examples are intriguing, but not universal proof: there is regional differences in regulation, availability, and what “approved” truly means.
Aesthetics is full of regulatory traps beyond exosomes: similar issues were raised around polynucleotides and other “skin boosters” (ingredient registration vs medical claims)
“Topical is one world. Injected is another.”
Not a member yet? Join the debate in the WhatsApp group
Longevity Docs is a highly vetted, invitation-only community for physicians shaping the future of longevity medicine. Apply to connect with our team.
NYC AI & Tech Mastermind
Small group. Curated. Limited to 150 Physicians only.
VIP - Includes private dinner with speakers
In-Person- Full access to all sessions and networking (10 tickets left)
Virtual - Live-stream and replay for those who can’t travel
Past, present and future perspectives on the science of aging
As Nature Aging celebrates its fifth anniversary, the journal asks some of the researchers who contributed to the journal early on to reflect on the past and the future of aging and age-related disease research, the impact of the field on human health now and in the future, and what challenges need to be addressed to ensure sustained progress. Nature Aging
10 key takeaways:
Epigenetic clocks transformed aging from an abstract concept into a quantifiable biological process, enabling intervention trials without waiting for disease or death.
Aging is neither purely random nor fully programmable, but a regulated, evolutionarily conserved process shaped by development and environment.
Longitudinal “pace of aging” measures are more clinically meaningful than single time-point biological age estimates.
Multiomics (especially proteomics) reveal that aging is organ-specific, heterogeneous, and systemically interconnected.
Immune aging is a central driver of multisystem decline and explains why lifestyle factors exert outsized effects on healthspan.
Partial cellular reprogramming proves aging is biologically reversible in principle, but remains experimental and not clinic-ready.
Aging mechanisms translate across species, but effect sizes shrink dramatically in humans due to biological and environmental complexity.
Most proposed geroprotective interventions show modest, variable, or transient effects in humans, underscoring the need for rigor.
The near-term clinical impact of aging science will come from risk stratification, prevention, and early intervention, not rejuvenation.
The credibility of longevity medicine depends on resisting hype, demanding human data, and prioritizing safety over speculation.
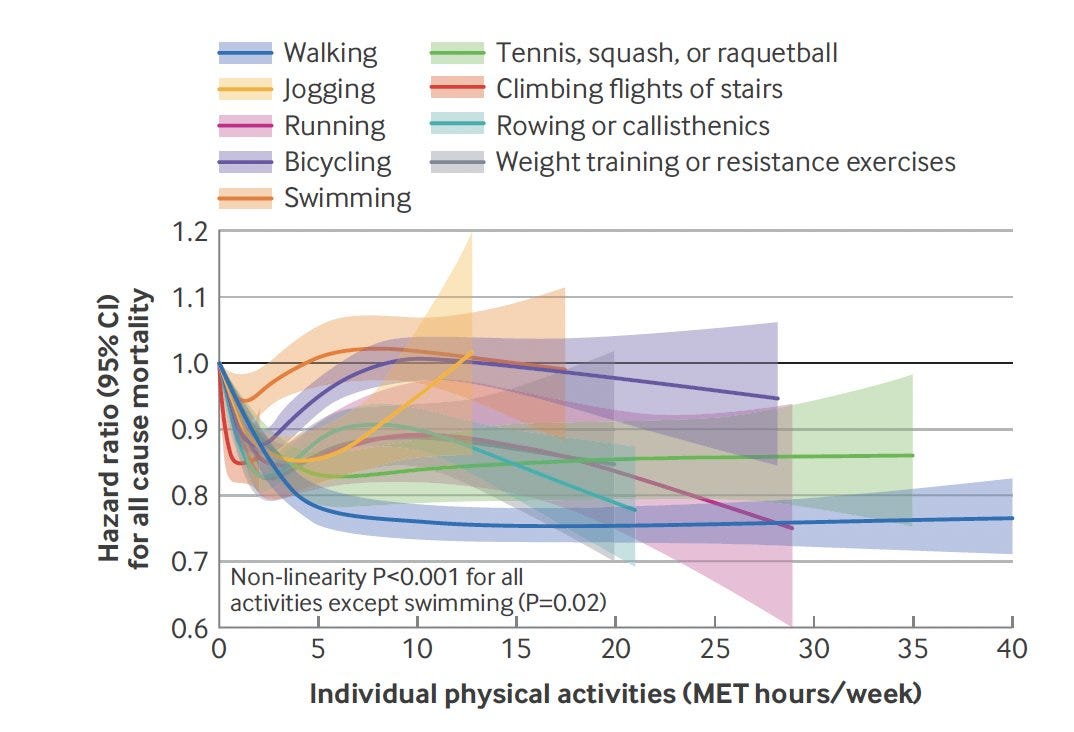
Physical activity types, variety, and mortality: results from two prospective cohort studies
Two big cohorts (Nurses’ Health Study + Health Professionals Follow-Up Study; ~111K healthy adults followed 30+ years) found that higher long-term total activity and most specific activities (walking, running, racquet sports, stairs, rowing/calisthenics, resistance training) were linked to lower all-cause and cause-specific mortality, with benefits that plateau at moderate doses; swimming was the main exception (no clear all-cause mortality benefit).
Crucially, people who consistently did a wider variety of activity types had lower mortality even after adjusting for total activity: the highest variety group had ~19% lower all-cause mortality and 13–41% lower CVD/cancer/respiratory/other deaths.
Bottom line: don’t just “move more”→mix it up; combining multiple activity types over years appears to extend lifespan beyond the benefit of total volume alone. BMJ
Every week, I track funding, FDA approvals, product launches, and breakthrough announcements shaping longevity medicine.
CARE
Your next primary care doctor could be online only, accessed through an AI tool
The NPR article describes how AI-powered, online-only primary care is emerging as a response to the severe shortage and burnout of primary care doctors in the U.S. Programs like Mass General Brigham’s Care Connect use AI to triage patients and support remote doctors, offering fast, 24/7 access for routine and urgent issues.
AI
Giving your healthcare info to a chatbot is, unsurprisingly, a terrible idea
The Verge article warns that sharing personal medical data with consumer AI chatbots like ChatGPT Health carries real risks, despite promises of privacy. Unlike doctors or hospitals, tech companies are not legally bound by healthcare privacy laws, and protections rely mostly on company policies that can change.
It also highlights the regulatory gray zone: these tools are widely used for interpreting labs and health decisions, yet avoid medical-device oversight by claiming they’re “not for diagnosis,” even as they project authority and personalization that users naturally trust.
AI health tools may be helpful, but trusting them with sensitive health data or medical decisions is premature until stronger regulation, accountability, and safeguards are in place.
WEARABLES
Ultrahuman and Click Therapeutics Partner on FDA-Authorized Migraine Tool
With the FDA-authorized Migraine PowerPlug, Ultrahuman and Click Therapeutics are moving beyond dashboards and into prescription-grade digital therapeutics, combining real-time biomarkers with clinically validated software. Most wearables observe, very few intervene. In practice, this signals a shift toward software-enhanced therapies where physiology, behavior, and treatment adapt continuously. Longevity docs should take note: the future standard of care will be hybrid: drug, device, and algorithm working as one.
BUSINESS
So You Want to Start a Concierge Medicine Practice? Here are Five Key Legal Considerations
Concierge medicine offers physicians more autonomy and deeper patient relationships, but it comes with significant legal complexity. Rules vary by state, and Medicare, insurance, and anti-kickback laws can easily be violated if the model is poorly structured.
Clear contracts, transparent pricing, and compliant marketing are essential to reduce risk. Always-on access, telemedicine, and AI tools increase privacy, data security, and liability exposure. Concierge medicine isn’t a loophole, it’s a redesigned medical practice that requires careful legal planning. Read more
SOCIETY
Longevity Gyms Start Packing a Punch
Longevity gyms are emerging as “gyms 2.0”, combining exercise with real-time data from labs, wearables, biomarkers, and AI to deliver hyper-personalized health and training guidance - not just workouts, but recommendations based on biology, stress, recovery, and lifestyle.
Driven by mainstream interest in longevity, AI tools, and consumer empowerment post-pandemic, these gyms (like Equinox, Sparkd by Chi Longevity, and Life Time’s Miora) are integrating medical-grade testing, coaching, and long-term monitoring to help people live better, longer.
The opportunity is big, but so are the challenges: higher costs, staffing and training shifts, data overload, and medical responsibility. Dr. David Luu argues gyms will need a Chief Longevity Officer as personalization becomes the norm. WWD
Connecting longevity talent with meaningful roles, collaborations, and impact.
Leadership & Clinical Roles
Miami Physician
A Miami-based longevity concierge startup is seeking a trained physician with excellent communication skills and bedside manner to support a highly curated concierge service. Must be based in Miami.
📩 Talent or opportunity to share? Contact us at contact@longevitydocs.org
Conferences
Longevitydocs AI & Tech Mastermind — January 31, 2026 (New York)
CALM — February 27–28, 2026 (Fort Lauderdale, FL)
Longevitydocs Summit, Cannes — June 9 – 11, 2026 (Cannes, France)
A4LI H-SPAN Summit D.C. (Alliance for Longevity Initiatives) — June 29 – July 1, 2026 (Washington, DC)
ARDD (Aging Research & Drug Discovery) — August 24-28 (Copenhagen, Denmark)
Longevitydocs Skin Longevity Mastermind — October 17, 2026 (New York)
Longevity Clinics Roundtables / Buck Institute — tba
Books
I wanted to share 3 upcoming books from Amy Shah, MD, Florence Comite, MD, and Michael Clinton. Excited for the community to keep educating and raising awareness
The Longevity Medicine Network
longevitydocs.™ is the world’s largest physician network in longevity medicine, serving 600+ vetted physicians across 50+ countries. We unite physicians, industry, and institutions to build the trusted global infrastructure that makes longevity medicine the new standard of care.
Longevity medicine is the personalized, evidence-based practice of modifying the root mechanisms of aging (biological, cognitive, and psychosocial) before they become disease, extending healthspan, not just lifespan. Using advanced diagnostics, precision interventions, and AI-enabled monitoring, it translates measurement into action across every medical discipline. Success is measured in functional capacity, vitality, and disease-free years.
Our Pioneering Approach: Uniting Science, Clinical Practice, and Culture
Professional Network
Global Longevity Community: A curated community of leading longevity physicians fostering peer learning, clinical collaboration, and professional growth
Medical Education
Certified longevitydocs.™ (CLD): The first structured, physician-led clinical curriculum for longevity medicine - comprehensive, evidence-based, and practice-ready.
Clinical Research
Longevity Research Network: Clinical research infrastructure enabling rapid generation of real-world evidence across the Longevity Docs network.
Cultural Experiences
Global Events: From Cannes to New York, our Summits, Awards, Masterminds, and Jefferson Dinners convene top researchers, clinicians, investors, and government officials to shape longevity medicine’s growth, investment, and policy.
Intelligence
Strategic Insights: Weekly syntheses of scientific breakthroughs, clinical best practices, business signals, and global market analysis for Fortune 500 companies - the industry’s trusted source of intelligence.
Not a member yet? Longevity Docs is an invitation-only network of 600+ physicians shaping the future of longevity medicine through clinical collaboration, certification, and global events.
Subscribe to the Longevity Docs Newsletter
Stay connected with a global network of 500+ physicians in 50+ countries advancing longevity medicine. Get evidence-based insights, clinical updates, and exclusive access to the community shaping the future of longevity care.
Newsletter Disclaimer: