2025 Longevity Medicine Recap: What Accelerated, What Broke
#76 Weekly Longevity Medicine Intelligence
Hey Doc,
This morning, I woke up reflecting, not just on my own year, but on ours as an industry. I’m grateful for the evolution. What changed since December 2024:
For us: we created a summit in Cannes. Launched a certification program. Built a research network. Went from 250 physicians to 600+ across 50 countries.
For the industry: i believed we matured as an industry… understanding that innovation and responsibility must grow together.
I truly believe that we underestimate what we can achieve in a year.
2025 taught us that lesson at scale. Here’s what actually happened.
Dr. David Luu - Founder, longevitydocs.™
PS: this is picture of my happy place.
Each week, I try to explore one idea that could advance longevity medicine and hopefully support physicians in bringing it to life.
Longevity Medicine 2025: What Accelerated, What Broke
When we started building in 2021, most people were still asking: “What is longevity medicine, exactly?” 2025 was the year longevity medicine escaped the clinic and entered society. Here’s what actually happened.
What Accelerated
1. Longevity became pop culture
Longevity moved from niche science to mainstream conversation. From Netflix to podcasts to beauty and fashion, longevity became an aspiration, not a stigma.
2. Longevity moved beyond clinics
Longevity showed up in gyms, hotels, corporate wellness, and homes.
Medicalized or not, consumers now access multi-tier solutions with very uneven evidence.
3. Clinics exploded
Longevity clinics multiplied fast, often faster than standards.
Access and visibility grew globally, but scale clearly came before standardization.
4. Biomarkers as a commodity
Blood tests, clocks, CGMs, and scans became affordable and mainstream.
Testing got easy; interpretation did not. Data moved faster than clinical judgment.
5. Startups bet on Longevity
Companies finally treated longevity as a real category. 2025 brought longevity EMRs, supplement, skin health, test, wearables, and full tech stacks for longevity care.
6. Education scaled fast
Conferences, certifications, and courses exploded. Demand for knowledge outpaced the field’s ability to ensure depth, rigor, and competence.
What Broke
7. The black market expanded
Peptides and hormones flooded grey markets as demand outpaced regulation. “Research only” became a label, not a safety standard.
8. Polypharmacy became normalized
Patients stacked GLP-1s, peptides, hormones, and supplements freely. Personalization often blurred into complexity without clear evidence or stopping rules.
9. Followers replaced credentials
Longevity became content, and authority fragmented. Reach sometimes mattered more than outcomes, and patients often heard influencers first.
10. The workforce gap became obvious
Doctors were asked to practice longevity medicine without being trained for it.
The bottleneck isn’t innovation: it’s education, judgment, and clinical standards.
The Real Takeaway of 2025
Longevity medicine didn’t fail in 2025. It scaled faster than its foundations. 2026 will be about standards, training, and restraint or let the loudest voices define it.
Next week: my 2026 predictions.
____
Join 600+ physicians across 50+ countries shaping the future of longevity medicine.
Apply to Join the Network | Learn About CLD Certification | Register for AI Mastermind
Every week, the Longevity Docs WhatsApp group feels like a front-row seat to the future of medicine. Here’s what had doctors buzzing:
The Consent Reckoning: When Optimization Meets Real Risk
(GLP-1s, peptides, stacking - and the patients we don’t expect to see in ICU)
One of the most sobering conversations this week came from physicians working in acute care.
Two “fit and well” patients.
Two life-threatening presentations.
Both under longevity-style optimization protocols.
The discussion wasn’t about blaming innovation it was about consent, contraindications, and responsibility in a field that’s moving faster than long-term data.
What doctors flagged:
Rare but real GLP-1 complications (bowel obstruction, ischemia, pancreatitis), especially in patients with prior GI surgery or adhesions
Polypharmacy by stacking peptides, hormones, and metabolic agents without fully understanding interactions
Patients who look healthy but have hidden risk factors (hematocrit, motility, vascular tone, arrhythmia risk)
The hardest truth shared:
“It’s not sexy, but long consent processes may be the most important intervention we have.”
Several clinicians emphasized visible risk disclosure, structured consent, and slowing down escalation, especially in the “well” patient where benefit margins are narrow.
Key Takeaway:
Longevity medicine will be judged not by its upside but by how it handles downside.
If we don’t lead on consent, contraindications, and restraint, others will define the narrative for us.
Peptide Regulation Shockwave: Demand Is Exploding, Standards Are Not
A short question: “Thoughts on the proposed peptide law?” opened a much bigger conversation.
Doctors quickly moved from curiosity to concern:
Supplier trust collapsing: multiple clinicians expressed hard stops on commonly used vendors
Increased awareness that many suppliers operate in a gray regulatory zone, often labeled “for research only”
Growing fear that poorly regulated access could trigger overcorrection by lawmakers
Several voices were blunt:
“Don’t use them.”
“Nope.”
Not because peptides have no future but because credibility requires discipline.
Key Takeaway: Peptides are no longer niche. They’re mainstream and that’s exactly why the bar must rise. The opportunity for physicians is not broader access, but clear standards around sourcing, indication, consent, and restraint before regulation is imposed from the outside.
Orthobiologics vs Surgery: “Don’t Treat the MRI, Treat the Patient”
A shoulder MRI case sparked one of the most practical, grounded clinical threads of the week.
The patient had a tear.
The MRI looked bad.
Surgery was being pushed.
But experienced clinicians slowed the conversation down.
What emerged:
Many partial rotator cuff tears heal with time, PT, and proper load management
PRP and biologics are best understood as modulating inflammatory imbalance, not magically “regrowing cartilage”
Imaging often overcalls severity, especially when not correlated with symptoms or ROM
Dynamic ultrasound, in expert hands, can outperform MRI for functional assessment
One line captured the spirit of the discussion:
“The most important technology is the doctor who sits between the imaging and the patient.”
Key Takeaway: Longevity medicine isn’t anti-surgery, it’s anti-reflex. Patients need clinicians who can interpret imaging through function, symptoms, and trajectory, not outsource judgment to a report.
Not a member yet? Join the debate in the WhatsApp group
Longevity Docs is a highly vetted, invitation-only community for physicians shaping the future of longevity medicine. Apply to connect with our team.
AI & TECH MASTERMIND | JANUARY 31, NYC
We’re bringing together 150 longevity physicians building AI-powered longevity practices.
If you’re still figuring out which AI tools are HIPAA-compliant, how to integrate wearables into clinical decisions, or whether proteomics is ready for practice, this is where you get answers from physicians already doing it.
What we’re covering:
Next-gen biomarkers (proteomics, epigenetics, multi-omics)
Wearables and continuous monitoring: clinical-grade vs. wellness theater
NeuroTech and brain aging protocols
Performance metrics that track biological age
AI imaging that catches what radiologists miss
Tech stacks that actually work (EMR integration, dashboards, APIs)
Clinical workflow tools: triage, documentation, protocol generation
AI-powered practice growth without physician burnout
The debate: frontier tech vs. what’s ready now
Your Monday morning action plan: 90-day implementation roadmap
Small group. Curated. Limited to 150 Physicians only.
VIP (50 spots) - Includes private dinner with speakers
In-Person (limited) - Full access to all sessions and networking
Virtual - Live-stream and replay for those who can’t travel
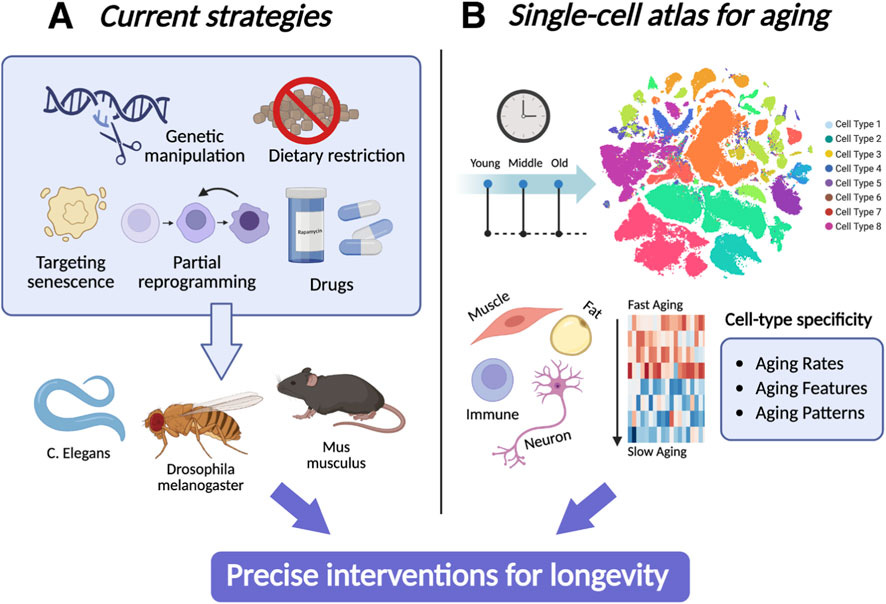
Toward precision longevity: aging interventions in the single-cell atlas era
This Frontiers mini-review reveals why longevity interventions work unevenly: different cell types age differently. Single-cell atlases are emerging as the missing layer that explains why the same intervention benefits some tissues but not others. The future of longevity medicine is precision aging, cell-by-cell, not one-protocol-fits-all.
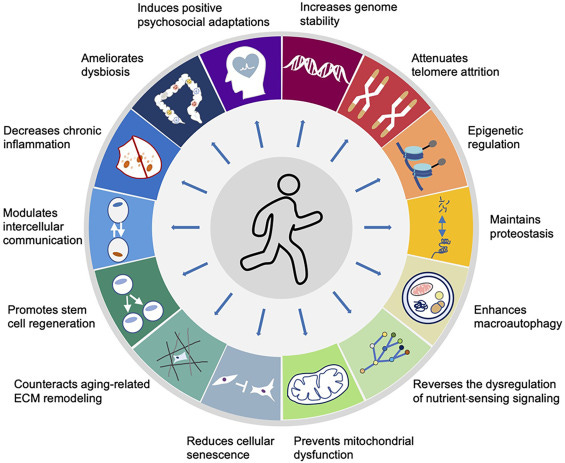
Exercise attenuates the hallmarks of aging: Novel perspectives
Exercise is still the most validated longevity intervention we have, especially for older adults. This review argues exercise may favorably influence all 14 hallmarks of aging, but admits a key gap: much of the “hallmarks” mechanistic evidence is still animal-heavy, and we need better human studies (tissue-specific effects, mtDNA, proteostasis/autophagy, nutrient sensing, ECM remodeling, telomeres).
Every week, I track funding, FDA approvals, product launches, and breakthrough announcements shaping longevity medicine.
AI/TECH
Noom Enters Longevity Medicine
Fitt Insider. The digital health company unveiled a diagnostics-driven microdosed GLP-1 program to preempt and reverse chronic disease - completing its evolution from diet app to full-stack preventative health platform.
PHARMA
Is Amylin the next obesity drug?
Pharma Voice. Amylin analogs are emerging as the next wave, promising similar or better weight loss with improved tolerability, especially in combination therapies. Big pharma is racing toward phase 3 data and approvals in 2026.
Obesity care is shifting from single drugs to multi-hormonal, sequenced metabolic therapy, raising the bar for clinical judgment, patient selection, and long-term safety standards.
People Are Already Taking This Unapproved New Weight-Loss Drug
Wired: Retatrutide - Eli Lilly’s triple-agonist (GLP-1, GIP, glucagon) -has shown striking phase II results (~24% weight loss), fueling a fast-growing gray market supplied by overseas manufacturers and “research chemical” sellers.
LIFESTYLE
From Room Service to Stem Cells: Inside the Rise of Longevity Tourism
Vogue Longevity is becoming a travel experience. What started in clinics is now showing up in luxury hotels offering diagnostics, recovery, hormones, and regenerative care. Hospitality is turning into a longevity platform.
SOCIETY
The Role of Doctors Is Changing Forever
New Yorker: Medicine is being unbundled. Patients now navigate health through influencers, DTC platforms, and AI. They often meet doctors only at the end to manage the fallout. Authority is no longer given. Doctors must reinvent themselves as trusted guides—building relationships, setting norms, and helping patients navigate a fragmented, algorithm-driven health system.
The world’s largest physician network in longevity medicine
longevitydocs.™ is the world’s largest physician network in longevity medicine, serving 600+ vetted physicians across 50+ countries. We unite physicians, industry, and institutions to build the trusted global infrastructure that makes longevity medicine the new standard of care.
Longevity medicine is the personalized, evidence-based practice of modifying the root mechanisms of aging (biological, cognitive, and psychosocial) before they become disease, extending healthspan, not just lifespan. Using advanced diagnostics, precision interventions, and AI-enabled monitoring, it translates measurement into action across every medical discipline. Success is measured in functional capacity, vitality, and disease-free years.
Our Pioneering Approach: Uniting Science, Clinical Practice, and Culture
Professional Network
Global Longevity Community: A curated community of leading longevity physicians fostering peer learning, clinical collaboration, and professional growth
Medical Education
Certified longevitydocs.™ (CLD): The first structured, physician-led clinical curriculum for longevity medicine - comprehensive, evidence-based, and practice-ready.
Clinical Research
Longevity Research Network: Clinical research infrastructure enabling rapid generation of real-world evidence across the Longevity Docs network.
Cultural Experiences
Global Events: From Cannes to New York, our Summits, Awards, Masterminds, and Jefferson Dinners convene top researchers, clinicians, investors, and government officials to shape longevity medicine’s growth, investment, and policy.
Intelligence
Strategic Insights: Weekly syntheses of scientific breakthroughs, clinical best practices, business signals, and global market analysis for Fortune 500 companies - the industry’s trusted source of intelligence.
Not a member yet? Longevity Docs is an invitation-only network of 600+ physicians shaping the future of longevity medicine through clinical collaboration, certification, and global events.
Subscribe to the Longevity Docs Newsletter
Stay connected with a global network of 500+ physicians in 50+ countries advancing longevity medicine. Get evidence-based insights, clinical updates, and exclusive access to the community shaping the future of longevity care.
Newsletter Disclaimer:












What a thoughtful and comprehensive recap; thank you for presenting this in such a clear, evidence-focused way! From a clinical perspective, longevity medicine is increasingly moving beyond fragmented “hacks” toward systems-level thinking that integrates metabolism, inflammation, circadian biology, and functional physiology.
I especially appreciate how you highlight both mechanistic insights and practical limitations. In clinical practice, patients are understandably eager for strategies that extend healthspan, yet the ongoing challenge is distinguishing early, plausible signals from robust, reproducible effects supported by longitudinal human data. Your recap strikes this balance well, recognizing promising areas such as exercise, metabolic optimization, and sleep regulation, while being transparent about where evidence is still evolving. Another point that resonates strongly is the emphasis on intervention synergy rather than isolated solutions. Biological systems do not operate in isolation, and our approaches to healthy aging shouldn’t either. Integrating lifestyle interventions, risk factor management, and targeted therapies, tailored to individual biology, is clearly where the field is heading, and that’s encouraging from both a clinical and patient-education standpoint.
This overview really helps bridge cutting-edge science with everyday clinical decision-making. It’s exactly the sort of pragmatic, grounded conversation we need more of in longevity medicine, for both clinicians and the people we care for.
Excellent synthesis of where longevity medicine sits right now. The distinction between scaling and foundation-building is key because growth without standards eventually becomes its own liability. The consent conversation around GLP-1 complications and polypharmacy stacking is something I've seen firsthand in ER settings where patients show up with unxpected metabolic cascades nobody anticipated. The gap between consumer demand and clinical training is only widening and that's where trust erodes fast.